
This research and more will be on show at the Chartered Association of Business School's Annual Research Conference on March 20 at the University of Edinburgh, which will be showcasing how business school research is delivering a positive impact on society.
As a business school academic it is not often possible to say that your research led directly to lives being saved. However, this was one particularly positive outcome of research conducted by myself and colleagues Nicola Burgess and James Hayton into knowledge diffusion and brokering in the English NHS.
In fact our work helped prevent moreF than 100 hip fractures and saved 60 lives according to the NHS Trust we worked with.
A research project in which we demonstrate how it is possible to overcome many of the barriers that prevent the spread of good practice from frontline services to other parts of an organisation and, in doing so, really make a difference.
In an ideal organisation, knowledge about good practice and good practice innovation would make its way from wherever it originates, often at the frontline of service provision, to the parts of the organisation where it is useful. Unfortunately, this is rarely the case. And, while in most organisations a failure to disseminate innovation and good practice might have a negative impact on profits, business development and competitiveness, in some organisations it can mean the difference between life and death.
This is certainly the case in healthcare provision. Yet, as our work on healthcare improvement with the Organising Heath Research Network shows, through comparatively small changes in approach it is possible to make significant improvements in patient safety.
Our study initially spanned a period of almost three years during which we endeavoured to develop a deep understanding of the effective dissemination of good practice information, from the people who possess that information to other parts of the organisation.
A number of key components were involved. First, there is the concept of knowledge brokering itself, the act of getting the right knowledge, into the right hands, at the right time. Often presented as a panacea for disseminating best practice within or across organisations our studies show that, in professional organisations such as hospitals, hierarchies of status and power prevalent in these professional bureaucracies present significant barriers to effective knowledge brokering.
In the context of knowledge brokering we looked at the role of the hybrid middle manager; these are managers who participate in both practice and management.
In our studies hybrid middle managers ranged from below executive director level all the way to ward managers and included: clinical directors and consultants who tend to head up and lead medical teams in different specialties; nurse managers, where they have responsibility for ensuring clinical governance, who typically work in concert with the clinical directors; and ward managers leading care delivery teams at ward level.
The extent to which the hybrid middle managers split between managerial and clinical duties varied. They may or may not directly deliver service on the ground, but are likely to be both clinically practicing and performing a managerial role. With a foot in both management and practice domains, hybrid middle managers are crucial brokers of quality improvement related knowledge within a health care provider, both upwards and downwards.
In investigating the role of hybrid middle managers in relation to knowledge brokering, we wanted to look at an issue recognised as important to the NHS, and relevant to the managers and clinicians involved in service delivery. We focused on the elderly and associated patient safety problem, and in particular fall incidence and prevention.
It is worth setting the context within which we looked at how hierarchies in the hospital, the source of our main findings, affected knowledge brokering.
The regulator monitoring the hospital's patient safety performance had criticised the trust due to the high incidence of falls and poor response in managing those falls. The clinical governance system is the mechanism through which this type of issue should be addressed, with ultimate responsibility resting with the chief executive.
However, our study revealed a process that tended to become characterised by a culture of entrapment. Criticism provoked defensiveness. The governance process ground to a halt, replaced by efforts to buffer the local organisation from regulatory pressure. An unhealthy response, but not uncommon in such circumstances.
Meanwhile, on the frontline in service delivery there were eight wards, all sited relatively near to each other, experiencing high levels of falls. Closer examination uncovered good examples of local innovation aimed at reducing the incidence of falls in one of these wards; good practice that would be useful to other wards and hospitals, trying to minimise the incidence of falls in elderly patients.
Older patients were put into cohorts, with a risk assessment of the likelihood of a patient falling. Patients most at risk of falling were put near to the nursing desk so that if they needed to move, to go to the toilet, for example, they would get a more immediate response from the nurses.
Yet, despite all eight wards suffering similar problems, and despite their physical proximity, that innovation was only disseminated to one other ward, and did not spread beyond that. This seemed surprising.
However, the reasons for the lack of dissemination became clearer when we interviewed staff who worked there, and reviewed the archive of documents and materials amassed during the study. Those reasons were rooted in the workplace hierarchies that existed.
How does a nurse manager overcome powerful hierarchies?
Take nursing, for example. In some ways the hierarchies in nursing are much like in the military. Hybrid nurse middle managers in clinical governance roles draw on their status and formal position in the organisation to influence nursing activity. Unfortunately it is that same status and formal position that discourages the nurses delivering frontline care from sharing their knowledge and ideas about improving patient safety in the care of older people.
The evidence showed that although senior nurse managers could make demands of ward managers and expect them to comply, ward managers could not take local innovation and knowledge and ensure that it reached further up the organisation by influencing senior nursing managers. Where good practice did reach one other ward it was due to the good personal relationship between the respective ward managers.
Nor were formal structures in place to ameliorate the powerful hierarchical effect. Hybrid nurse middle managers had to resort to the nursing equivalent of managing by wandering around. These "patient safety rounds" were intended to circumvent hierarchy and access knowledge held by junior staff.
Hierarchy also affects the dissemination of knowledge between medical professionals where the issue is predominately one of status. This was evident in doctors. As one doctor said: "Some [doctors] are more equal than others".
Take geriatricians, who commonly interact with their peers across many clinical departments where older patients are located. They deliver holistic care, are more involved with the patients than most doctors would be, and are well positioned to possess knowledge concerning patient safety improvement.
However, geriatricians are also considered to be comparatively low status by other medical specialities, such as surgeons or anaesthetists, for example, and therefore find it difficult to influence their peers regarding the adoption of new practices.
Whereas our evidence suggests that those medical specialists that have high status and would be able to bring about changes are not motivated to do so. They do not see patient safety as their concern, indeed many believed it to be the domain of nurses. So much so that some even refused to attend patient fall related meetings or engage in relevant governance processes. This attitude persists, even though the specialist wards invariably have significant numbers of elderly patients.
And there was the interactions between nurse middle managers and doctors, what is known as interprofessional hierarchy. Differences in the routes into the respective professions, reinforced by elitist attitudes across hospitals that medical professionals are more important than nurses, makes brokering of knowledge from nurse to doctor difficult.
Again, many specialist doctors, other than geriatricians, tend to view patient safety as being the responsibility of nurses, and outside the compass of their role.
Both nurse managers and doctors have clinical and managerial roles, with their clinical service role impacting on the incidence of falls. The professional and managerial elements of the organisation needed to mesh and work together to be effective.
But while we found that there was not necessarily tension between the two, our findings did show that the two are decoupled, managerial governance systems were not tightly enough linked to service delivery. For example, we found evidence that where there was a Serious Untoward Incident (SUI) and nurse managers were progressing governance procedures, doctors were reluctant to get involved beyond signing forms.
While our studies revealed power and status barriers that were interfering with the effective transmission of best practice knowledge, they also suggested possible methods of removing or circumventing these barriers.
We uncovered examples of hybrid middle managers taking positive steps to ensure that information about 'falls best practice' was disseminated from nursing staff to the highest levels of the organisation.
From the hours of interview transcripts we were able to piece together insights from the frontline in order to understand what HR practices might help mend the broken chains of knowledge. And, in doing so, create a better environment for ensuring that safe care is delivered to older people.
Evidence from interviews suggested that bringing people together, including frontline staff, hybrid-middle managers, and where possible senior management, creates opportunities for interaction and knowledge sharing, upwards and laterally, that might not otherwise take place.
This might be through monthly multi-disciplinary team meetings, for example, which can incorporate issues on wards, present serious incidents of patient falls, and discuss ongoing governance procedures. Or there may be specific structures set up to tackle a particular issue, such as falls.
Although the organisation of clinical practice might fail to provide opportunities for individuals to broker knowledge upward to higher-status clinicians, motivated individuals can step in to create opportunities to champion and influence change.
Take the situation where one geriatrician set out to educate peers about the importance of proactive fall prevention for patient safety. In doing so they were careful to frame the issue of fall prevention as relevant right across the organisation - to young patients, new mothers, cardiovascular patients, and stroke patients - and not just as a matter pertinent to the care of older people.
Related course: Executive MBA with Healthcare Specialism
At the same time they leveraged social capital acquired over 30 years of practice to co-opt a senior nurse occupying the hybrid middle manager role of clinical quality, risk and safety manager, into prioritising falls as an organisation-wide issue.
"Champions" can also promote more effective knowledge brokering by influencing future generations of medical professionals. We discovered examples of early career intervention where a geriatrician focused on educating junior doctors in basic patient safety practices, emphasising the "team" role of doctors working alongside nurses.
He explained to us that this increased the motivation of doctors to engage with patient safety knowledge and activity because it routinised patient safety behaviours and encouraged those exposed to this kind of advocacy to pass on behaviours to other doctors.
There was evidence too that doctors did not necessarily feel comfortable in or adequately prepared for the managerial element of their role. With nurses there is an observable career progression of nurse to ward manager, to matron and beyond, facilitating a gradual evolution of managerial status, aligned to experience.
Ultimately this serves to empower hybrid nurse middle managers to influence practice for patient safety improvement. However, managerial identity remains an issue for doctors when positioned in hybrid middle manager roles, suggesting that they would benefit from greater learning and development opportunities focusing on this aspect of their role.
The importance of effective performance management and targets were also highlighted, especially in a professional context where considerable emphasis is placed on evidence-based decision making and meeting targets.
In one case, for example, data was available on fall incidence and the immediate consequences of those falls, but not on long-term consequences. It was impossible to analyse links between initial falls and eventual deaths. Capturing that data enabled the team to construct more accurate risk scores for falls and initiate data driven action as a result.
Thus, our studies highlighted possible HR mechanisms, such as job designs, performance management systems, and training and development interventions that could create opportunities for knowledge brokering interaction, and motivate individuals to engage.
How to cut elderly patient falls in hospitals
An important part of our work involves stepping into the medical practitioners' world, relaying our findings, and working with them in a practice setting, to implement changes that will improve existing practices. Note that we do not seek to impose solutions.
We may suggest solutions to improve knowledge brokering, for example, but we recognise that those solutions need contextualising. It is the people working in the hospitals who are best able to identify how those solutions might be translated into practice and implemented.
Prior to our intervention the process following a fall, as we observed it, was as follows. If, for example, an elderly person falls over on the ward and fractures their hip, this is recorded as a SUI; an incident which results in unexpected or avoidable death, or moderate or serious harm to a patient. This triggers a Root Cause Analysis (RCA) report which includes an action plan for improvement; the RCA is presented to a clinical risk committee, typically by the relevant ward manager.
Then what tended to happen was one (or several) of three things. The incident would be dealt with in a relatively tokenistic way, a tick-box exercise going through the motions to satisfy the patient, patient carer or relative. Or everyone might conclude that it was a systems failure, and not something that anybody could really do anything about. Or a member of staff, usually the ward manager, would end up having the blame pinned on them. Which, unsurprisingly, created an extremely defensive culture.
What tended not to happen were any remedial measures being acted upon, or any suggestions included in the action plan actually implemented. Regardless of the elaborate mechanisms and processes in place to deal with SUIs and despite there being a formal mechanism designed to elicit knowledge sharing and brokering, you got compliance at best. It was a governance system that had blame embedded in it.
During our study we provided the clinical governance committees at the hospitals with regular reports, both in written form and verbally, on our findings. Having done that, we started working with the NHS Trust staff to co-produce solutions.
The challenge was to implement measures that would lead to learning and service improvement. We suggested a number of initiatives to help improve the knowledge brokering and dissemination of good practice.
We took each of the eight wards involved in turn, and gathered as many people together as possible who were associated with that ward and fall prevention. The aim was to spend time discussing how issues relating to falls prevention could be addressed. What was the learning in service improvement? What are the types of innovation that could be diffused? These were two to three hour meetings.
The meetings were held in a learning centre and facilitated by our research team. Spaces are very important to organisations. The routine clinical practice is a professional space. In that space, the usual hierarchical norms of behaviour that were discouraging knowledge brokering would be in operation.
However, the learning centre was seen as a neutral space. It allowed us to get all of the various teams together, and facilitate what are quite emotionally laden interactions. With surgeons, geriatricians and nurses together, without facilitation you would be unlikely to hear every voice.
In the normal work environment nurses might typically have acquiesced to the views of doctors, for example, not said anything, and then afterwards discussed it among themselves. When that happens their insights are lost. In our meetings, nurses were allowed to have a voice and surgeons listened in a way that suspended what would typically be expected in day-to day-practice.
It is also worth noting that beyond the relational, hierarchical aspect of the facilitated meeting in a neutral space, there is also a reputational element in action. Because when doctors talk to clinical teams in front of their peers, and other associated professionals, they do not want to be seen as dismissing patient safety and the measures that might be taken to improve it.
For example, those surgeons that might otherwise dismiss patient safety as someone else's domain, would want to be seen as caring and at the cutting-edge of the profession in terms of innovation, as that perception has an impact on their reputation among their peers and others.
The group meeting or focus group also allows for educational intervention. It provides an opportunity to engage evidence driven medical professionals, such as surgeons, by presenting them with audit data, with evidence about the incidence of falls, where there had been interventions, and how those interventions had led to a decrease in the incidence of falls.
How to put in HR practices to prevent elderly patient falls
Our work in the group meeting dealt with the professional organisation – the wards and other associated medical professionals delivering the care. However, a second key aspect of our work in the NHS Trust was our engagement with the managerial organisation in the hospital, specifically the clinical governance committee.
On governance our studies have revealed two significant flaws in existing practice. At present the climate within which the governance process took place left people feeling that they were on trial and therefore promoted defensiveness and reduced the prospects of knowledge dissemination.
This climate needed moderating, which would involve subtle changes in the ways in which the clinical governance committee interacted with the ward manager and deputy ward manager and other team members at ward level.
The other flaw that we detected in the governance process was that action plans developed as a result of RCA were rarely followed up, either to see if action had been taken, or whether it worked. Therefore, if it did work there was no diffusion of learning. Although this was partly a product of the volume of work at the hospital we made some suggestions for improving the governance process.
Working with the clinical governance structure we supported the development of a specific clinical governance sub-committee called the Falls Operational Group (FOG) and worked with them on following up action plans, service improvement, and diffusion of learning.
The composition of the FOG was particularly important as it was formed from a group of clinical champions, who were also opinion leaders, which meant that they were able to influence their peers towards better practice. Another key element was getting the chief executive to chair the group and bring their authority to it.
In many organisations there are middle managers who have both a managerial and service delivery role. These middle managers play a vital role in disseminating knowledge within the organisation. At the same time, particularly in professional organisations, hierarchies of power and status within the workforce can inhibit the ability or motivation for these middle managers to prevent the spread of good practice and innovation.
Our work shows how certain relatively simple HR measures such as facilitated group meetings, and the involvement of issue "champions", can help circumvent barriers to the dissemination of learning. Even awareness of the issues surrounding hierarchies is useful.
When such measures are taken it can have a significant effect on organisational performance. And, in the healthcare sector, as this comment from a geriatrician in the NHS Trust that we worked with confirms, it can be the difference between life and death.
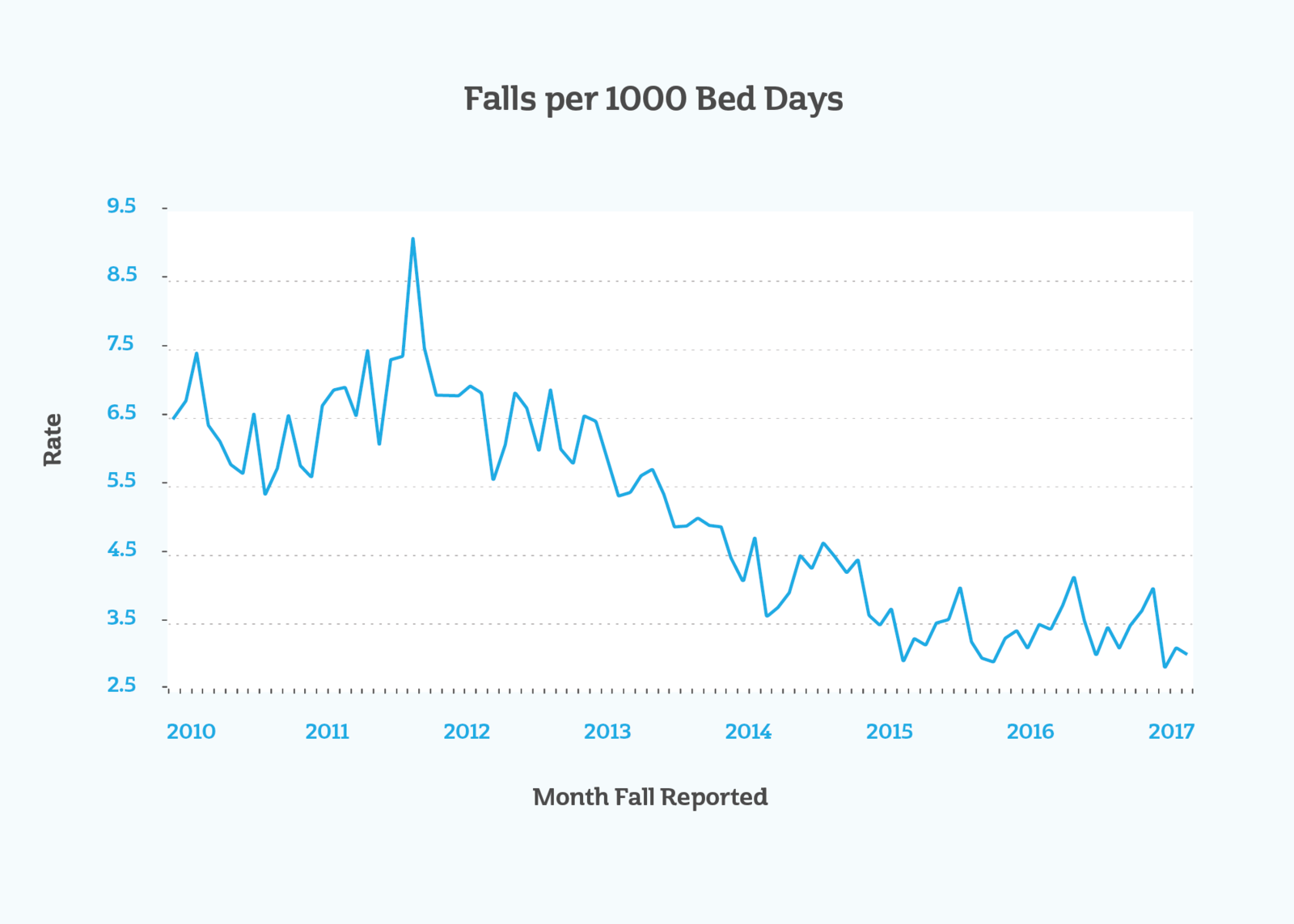
"The improvement work of which your project has been a part of has seen a dramatic reduction in harm to our inpatients as a result of falls," they wrote. "Since 2011/2012 we have halved the rate of inpatient falls, prevented over 100 hip fractures and saved 60 lives."
Graeme Currie is Professor of Public Management and is part of the National Institute for Health Research.
See this research on display at the Chartered Association of Business School's Annual Research Conference.
For more articles like this download Core magazine here.
To register for our healthcare newsletter click here.




 X
X Facebook
Facebook LinkedIn
LinkedIn YouTube
YouTube Instagram
Instagram Tiktok
Tiktok