Missed doctor appointments are estimated to cost NHS England £216 million a year; from 2014 to 2015 the NHS spent some £6.1 billion on overweight and obesity-related ill-health, a figure predicted to rise to £9.7 billion by 2050; while alcohol-related harm costs the NHS in England an estimated £3.5 billion every year, with alcohol-related admissions to hospital having grown almost 20 per cent over the last decade.
Meanwhile, a combination of factors - people living longer, more medical solutions, the state of the economy - mean that the NHS and many other healthcare systems around the world are under severe cost pressures. Yet, despite a constant drive to improve, considerable inefficiencies remain in the system.
As the evidence shows, people make poor and costly choices, whether it is not showing up for an appointment, eating an unhealthy diet, or having poor drinking habits, even when they are equipped with information that should allow them to make more sensible decisions.
If we want a healthcare system to operate in an effective and efficient way then we also need the people within that system - the public, patients, managers, or specialist practitioners - to act in the most efficient and effective way. To follow evidence-based practice. To make the "right" decisions.
Traditionally, the rational choice model has been used to influence people to behave in desirable ways. The assumption being that humans are rational beings, and if they are provided with the necessary information, they will rationally act in their own self-interest. Unfortunately, it is clear from the evidence that, despite apparently well-founded theory, this approach does not appear to work that well in practice.
Fortunately, a new approach to influencing behaviour - popularly known as 'nudge' theory after the book Nudge by Nobel prize-winning economist Richard Thaler and law school professor Cass Sunstein - provides policymakers with another option.
Nudge has become synonymous with the use of relatively low cost behavioural change techniques to influence behaviour and decision making, and builds on the work of Nobel prize-winning psychologist Daniel Kahneman, Thaler, and others in the behavioural science field.
This new approach has changed the debate about decision making, arguing that you cannot stop people being irrational because much of human decision-making is outside conscious awareness.
We frequently make decisions, almost instantaneously, influenced by the context and the environment. Why not go along with human nature, allow people to behave naturally, but seek to influence their natural decision-making impulses in order to produce outcomes beneficial for both the individual and society?
Policymakers have been quick to latch onto the possibilities. The UK Government led the way, setting up the Behavioural Insights Team, popularly known as the Nudge Unit, and other governments around the world have since followed suit.
I was involved early on in helping to provide a framework which practitioners could use to understand and guide their use of behavioural change techniques. At that time the application of nudge was relatively random and inconsistent. It was clear at an early stage that policymakers and others who wish to apply nudge principles without having to become a psychologist or behaviourist, would need a more comprehensive and consistent checklist or framework.
The result was the MINDSPACE framework, published in 2010, a simple tool that can be used to diagnose problems and create interventions without being a behavioural expert. The report played an important part in helping to make the case to establish the Behavioural Insights Team. It set out nine of the most robust influences on our behaviour, captured in the simple mnemonic – MINDSPACE.
Healthcare is one area where nudge interventions should be able to make a difference. As a result, for several years, together with other colleagues, I have been testing the efficacy of nudge interventions in a number of different settings.
Nudging behaviours in healthcare: improving hand hygiene
So what does nudge look like in a healthcare environment? A good example is a study on reducing healthcare associated infections by improving hand hygiene compliance.
Healthcare associated infections (HAIs) are a significant cause of illness and death within healthcare settings, and financially costly both to patients and the healthcare system. Ensuring hands are kept sufficiently clean is key to preventing healthcare associated infections.
However, hand-washing compliance rates are often very low. One review identified compliance rates among healthcare providers of less than 40 per cent, in a study of visitors passing through a hospital lobby the figure was less than 12 per cent, while in our study only 15 per cent of baseline entrants to an intensive care unit (ICU) washed their hands.
Many initiatives have been tried to improve this and have been largely information-based, but have resulted in only transient and modest improvements.
Our research investigated whether psychological priming might provide a nudge to improve compliance rates. Psychological priming is where exposure to certain cues, such as words, smells, or images, changes a person's behaviour without them being aware of the impact of that cue.
In this case, prompted by studies demonstrating that individuals are more likely to keep their surrounding environment clean when primed with scent, we tested whether an olfactory prime - a 'clean' citrus smell - might improve hand hygiene behaviour at an ICU at a teaching hospital in Miami.
We also tested a visual prime, in the form of a photograph of a pair of eyes positioned above a hand gel dispenser to introduce a perception of being watched.
The study showed that the citrus smell (from an air freshener positioned nearby) was associated with a dramatic increase in hand hygiene compliance from 15 per cent in the control group to 46.9 per cent.
The male eyes also produced an increase from 15 per cent to 33.3 per cent. (The female eyes image had no impact). Consequently, the trial results suggest that considerable improvements are available by deploying a very modest and low cost behaviour changing nudge.
Nudging for health: reducing alcohol consumption
Excessive alcohol consumption places a huge strain on the NHS. In 2016/17 there were an estimated 337,000 alcohol-related hospital admissions, for example.
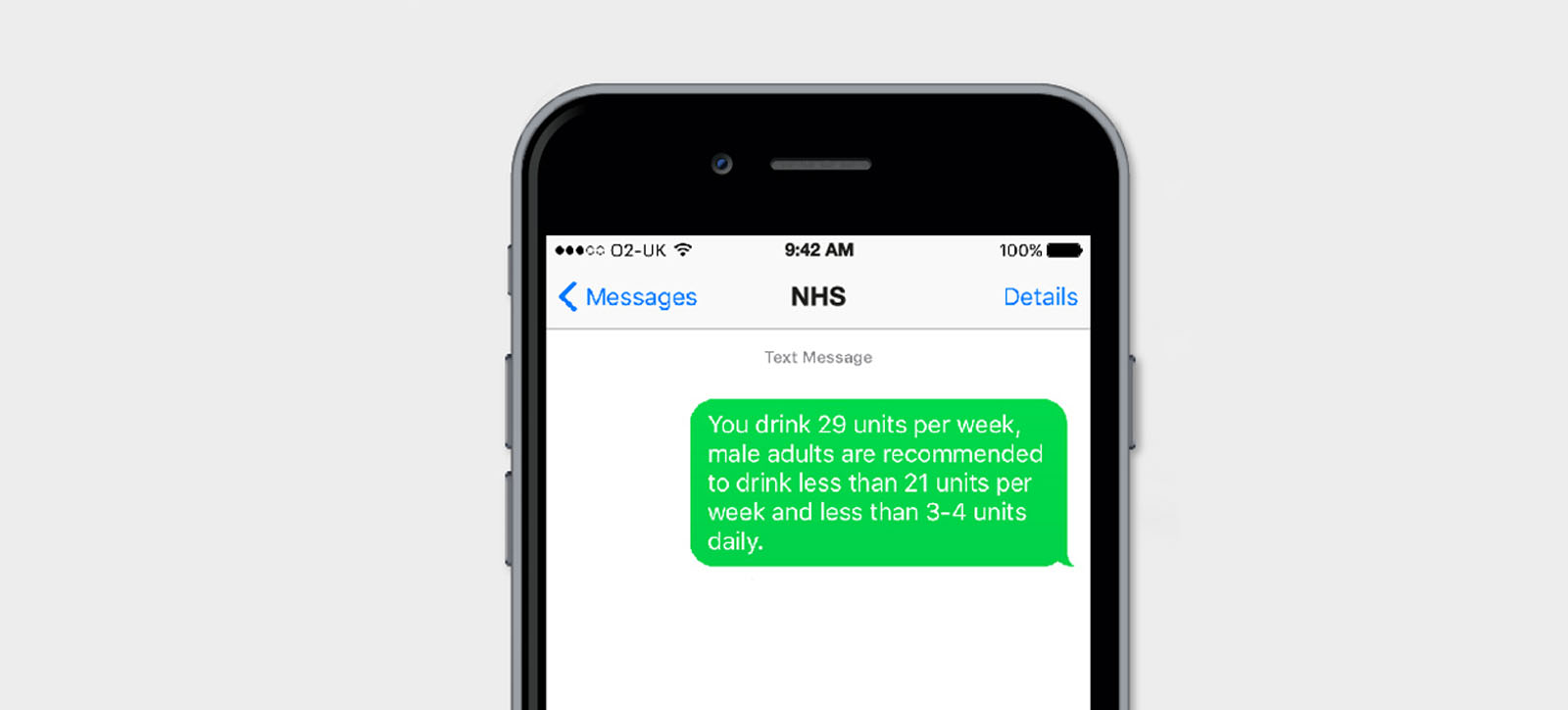
So in another study, we looked at ways of increasing awareness about the problems associated with this major public health issue. In particular, we tested an intervention designed to improve engagement rates with an online screening and brief intervention developed by UK-based alcohol awareness charity, Drinkaware.
Public awareness messaging about the effects of consuming too much alcohol is usually based on the long-term health effects. However, we decided to test whether framing the message around the short-term effects of excess alcohol consumption on appearance might produce better results.
Visitors to the Drinkaware website were greeted with a banner advertisement saying: "Are you drinking too much?" followed either by "Is this affecting your health?" or "Is this affecting your appearance?".
The aim was to encourage visitors to click through to complete an alcohol consumption screening tool, and then be forwarded on to further resources depending on their screening score.
We discovered that framing the message around appearance was a more effective way to encourage engagement with and completion of the screening tool, than focusing on health. This was even the case with users who achieved higher risk scores on the screening exercise, a group we originally believed would be more responsive to health-framed information.
Behavioural insights in healthcare: reducing costs in missed appointments
Another area where nudge has proved to be effective in healthcare is in the reduction of missed appointments. Missed appointments are a waste of resources, they are estimated to cost NHS England £216 million a year. An amount that it is stated could pay the annual salary of some 2,300 full-time family doctors.
We conducted two randomised controlled trials testing the impact of a re-worded reminder on ‘Did Not Attend’ (DNA) rates. In an initial trial of 10,000 patients, a reminder text message, sent in advance, that highlighted the cost of a missed appointment to the health system produced a DNA rate of 8.4 per cent, compared to 11.1 per cent for the existing message.
In a second trial of some 9,000 patients, a similar DNA rate of 8.2 per cent was observed, but a reminder referring to the cost of missed appointments in more general terms was significantly less effective.
The findings showed that missed appointments could be reduced significantly, for no extra cost, just by rephrasing the appointment reminder message in a more persuasive way. Indeed, switching from the existing message to the most effective cost-related message would mean close to 6,000 fewer missed appointments per year in the NHS Trust where we conducted the studies.
Yet another study focused on the public health challenge of tackling obesity, an issue which costs the NHS some £6 billion a year. Child obesity is a particular problem in the UK, with almost a quarter of four to five year-olds overweight or obese, and a third of all 10-to-11-year-olds.
Given that children with obesity are at greater risk of developing diabetes, heart disease and some cancers over their lifespan, these figures represent a significant health concern and potential future cost to healthcare systems.
The National Child Measurement Programme (NCMP) sent letters to the parents of overweight 10-11 year-old children in three English counties. The letters provided feedback on the weight of the children, encouraged healthy lifestyle behaviours, and provided an opportunity for parents to obtain weight management services for their children, if available.
However, evidence suggested that these letters could be more effective in prompting behaviour change. In one study, for example, although 72 per cent of parents expressed an intention to change their child's lifestyle, only 55 per cent reported such behaviour change in a follow-up survey, and only a third sought further information and support for their child's weight from the health professionals recommended in the NCMP letter.
Related course: Executive MBA Healthcare Specialism
We devised and tested an enhanced version of the letter, which we changed in a number of ways. In particular, we tried to help parents objectively recognise when their child was obese, and make it easier for them to enlist help to deal with that.
The enhanced letter included a visual aid showing computer-generated images of children's body shapes across different weight categories, as well as social norm information describing how a child's weight compares to others, and for very overweight children, a pre-completed form for weight management services.
Response rates were lower from parents of obese children compared with those of overweight children. Nevertheless, the enhanced letter approximately doubled uptake of the weight management services programme compared to the national template letter which was being used at the time of trial.
Our studies show that behavioural change techniques have an important role to play in shaping the behaviour of all those who interact with healthcare services for the better.
It is also important to add, however, that not any or every nudge intervention will create the desired impact. Implementation is key. The impact and success of any intervention or policy is determined by its implementation. Even a brilliant intervention badly implemented is likely to fail.
Trial design, the fidelity of any trial, trial management, all these are difficult challenges. Ideally, every organisation would have a Chief Behavioral Officer, as this would increase the chances of behavioural science thinking being embedded into the organisation. However, we are not there yet.
This is why the MINDSPACE tool was created. It is also why, with colleagues, I have helped to develop Intervention Design Worksheets, which we use in workshops, that detail a methodology to help people implement nudge effectively.
How to use nudge interventions in healthcare
And for those managers who want to trial nudge interventions but are not sure where to start, I would recommend applying systems thinking to their environment to ceate a map of causal relationships, understanding the relationships between behaviours and outcomes within their system.
Invariably, managers know about the financial position, about productivity, the economic impact of various decisions, and numerous other metrics that measure how the organisation works and performs, in order to meet their goals and strategies.
It is advisable, however, in addition to all this information, and especially in complex organisations such as the NHS, that managers have a greater appreciation of the effects of behavioural impacts within the system. That they are able to look at the organisation through the lens of behaviour and behavioural impact.
Further reading:
Schmidtke, K., Aujla, N., Marshall, T., Hussain, A., Hodgkinson, G. P., Arheart, K., Martin, J., Birnback, D. and Vlaev, I. (2017) "Using environmental engineering to increase hand-hygiene compliance : a cross-over study protocol", BMJ Open.
Kulendran, M., Vlaev, I., Gamboa, P. and Darzi, A. (2017) "The role of impulsivity in obesity as measured by inhibitory control : a systematic review", Medical Research Archives, 5, 8
Taylor, M. J., Vlaev, I., Maltby, J., Brown, G. D. A. and Wood, A. M. (2015) "Improving social norms interventions: rank-framing increases excessive alcohol drinkers’ information-seeking", Health Psychology , 34, 12, 1200-1203
Ivo Vlaev is Professor of Behavioural Science and teaches Mobilising Resources and Incentives for Healthcare Innovation on the Executive MBA Healthcare Specialism.
For more articles like this download Core magazine here.




 X
X Facebook
Facebook LinkedIn
LinkedIn YouTube
YouTube Instagram
Instagram Tiktok
Tiktok