
The NHS and Virginia Mason Institute Partnership has valuable lessons for healthcare leaders
This is the first in a series of six lessons on building a culture of continuous improvement that are relevant to every organisation in healthcare.
I’m hoping to foster a global conversation about how to lead continuous improvement within and across healthcare settings.
Each lesson will be followed by a ‘tweetchat’ on Twitter hosted by WBS in partnership with the #QIhour network. The lessons are summarised in Six key lessons from the NHS and Virginia Mason Institute partnership.
Following a competitive selection process, five National Health Service (NHS) hospitals were selected to take part in a five-year partnership with the US-based Virginia Mason Institute, known as the NHS-VMI Partnership. The goal was to develop a sustainable culture of continuous improvement.
These five hospitals adopted the same leadership infrastructure, the same training programme, and the same improvement routines and methods, yet the level of traction among doctors, nurses, managers, and senior leaders varied greatly, as did performance outcomes and the pace of change.
So how can we explain these differences of receptivity and performance, and what can we do to prepare the ground for a culture of continuous improvement to take hold?
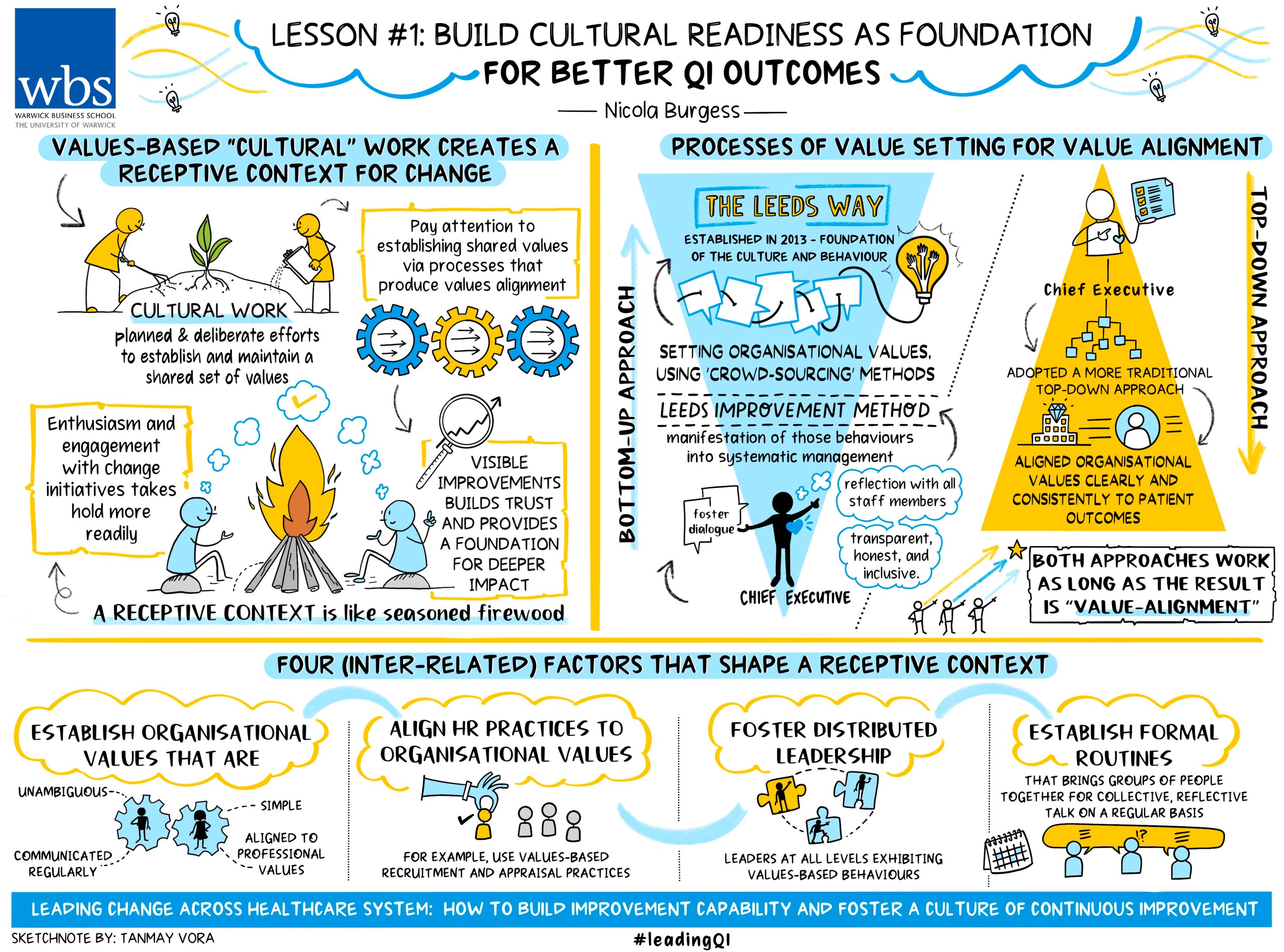
Values-based ‘cultural work’ creates a receptive context for change
I’ve coined the term ‘cultural work’ to describe planned and deliberate efforts to establish and maintain a shared set of values that all organisational members align to.
Organisations that engaged in values-based cultural work in the years prior to the NHS-VMI Partnership produced a more receptive context for change.
The difference between a receptive and unreceptive context can be likened to the difference between seasoned and unseasoned firewood.
Damp firewood is hard to ignite, produces smoke and ultimately damages the environment. Shortly after being lit any flames will smoulder and die, leaving traces of black toxic residue. (This residue a metaphor perhaps for the change fatigue or ‘initiativitis’ observed in organisations with a history of poorly understood, poorly executed and subsequently short-lived change initiatives).
By contrast, a receptive context is like well-seasoned firewood: enthusiasm and engagement with change initiatives are easy to ignite and grow steadily as improvements (no matter how small) are celebrated, while trust in the organisation’s continued commitment fuels deeper and longer lasting impact.
In sum, a receptive context is a fundamental resource for building the capability to improve and nurturing a culture for continuous improvement. To this end, I propose healthcare organisations wishing to nurture a receptive context should pay attention to values-based cultural work.
Focus on values: Processes of value setting for value alignment
Two of the five hospitals in the trial stood out for their consistent, uncontested, and unambiguous ‘values-based’ ethos established in the years prior to the NHS-VMI Partnership.
‘The Leeds Way’ was established in 2013 through a bottom-up approach to setting organisational values, using crowdsourcing methods.
Leeds Teaching Hospitals NHS Trust CEO Julian Hartley emphasised The Leeds Way was the foundation of the culture and behaviour, while the ‘Leeds Improvement Method’ (the routines and practices associated with developing the organisation’s continuous improvement capability and culture) represented the manifestation of those behaviours into systematic management.
He said: “The Leeds Way was created through a process of bottom-up engagement, [starting] with the moment of catharsis where people were able to describe how bad it felt to work here and we publicised and talked about that.
“We used a technique called crowdsourcing, which every one of our 18,000 staff had the opportunity to feed into, to say what they thought we should be doing, and how we should be working, and they could all see each other’s comments and vote on the best ones. And so, the wisdom of the crowd led us to The Leeds Way.”
This bottom-up approach enabled a then new CEO to foster dialogue and reflection with all staff members in a manner that was transparent, honest, and inclusive. Ultimately, The Leeds Way became embedded in the organisation prior to the partnership and embodied a shared set of values that all staff were aligned to.
By contrast, at the beginning of his tenure, Michael Wilson CBE, CEO of Surrey and Sussex Healthcare Trust (SASH) from 2010 to 2021, adopted a more traditional top-down approach to setting values.
He aligned organisational values clearly and consistently to patient outcomes. The rationale? He said: “The patient is the one consistent thing that everybody’s got in common. It’s the one reason why we’re all here and if you keep framing it in that way you can’t really lose."
At interview, Mr Wilson explained how clarity and constancy of the organisation’s values was central to the organisation’s way of working.
He said: “If you talk to the doctors here, they’ll say to you ‘well, [the CEO] only ever talks about four things’. I used to get all [senior doctors] in a room and say ‘well, you’ve got to do a lot of stuff, but I want you to focus on four things. Just four things, that’s your job. And for these four things you took an oath and that’s it.
“Spend all your time on patient experience, on quality, patient safety and getting the best clinical outcomes’ and they’d look at me and say, ‘is that it?’ and ‘you’re not going to talk about 90 per cent [waiting time target]?’ No, I’m not because I know that if you focus on those four things that’ll just happen.”
Cultural work produces cultural change
SASH presented one of the most striking illustrations of the foundational importance of cultural work. In 2010 SASH was “the worst performing hospital in the country on every single measure” according to Mr Wilson.
Shortly after Mr Wilson’s arrival in 2010 SASH found itself at the centre of Channel 4 documentary Dispatches, after secret filming exposed levels of care and compassion falling far below expectations.
Fast forward to 2019 and SASH became one of a small number of NHS trusts to be rated ‘outstanding’ by England’s independent hospital inspector, the Care Quality Commission (CQC). Furthermore, the CEO commented that many of the staff working at SASH in 2010 still work there today.
In its report, the CQC made multiple references to “an exceptional culture of data-driven continuous improvement and transformation at the trust…supported by a comprehensive meeting structure and detailed performance reporting processes”.
This resounding statement was testament to the adoption of routines, practices and an infrastructure for improvement via the NHS-VMI Partnership.
Based on this learning, I would highlight four (inter-related) factors that shape a receptive context:
- Establish organisational values that are simple, unambiguous, aligned to professional values and communicated regularly. (The examples of Leeds and SASH show that this can be done via a top-down or bottom-up process. The important take-away here is that organisational values must align with professional and clinical values).
- Align HR practices to organisational values (for example, use values-based recruitment and appraisal practices).
- Foster distributed leadership (leaders at all levels exhibiting values-based behaviours).
- Establish formal routines that bring groups of people together for collective and reflective talk on a regular basis. (Read more about how formal routines can achieve informal, collective and reflective talk here).
Each of these four factors are described in more detail in the evaluation report; I have focused on the first of the four factors: values alignment.
The first tweetchat will be held on Tuesday January 31, 7-8pm. Follow the hashtags #LeadingQI and #QIhour to join and learn more from the NHS-VMI Partnership.
Nicola Burgess is Reader of Operations Management and teaches Operational Management on the Distance Learning MBA plus Digital Innovation in the Healthcare Industry on the Executive MBA.
Follow Nicola Burgess on Twitter @DrNicolaBurgess.
More lessons from the Virginia Mason Institute – NHS Partnership:
1 Build cultural readiness as the foundation for better QI outcomes
2 Embed QI routines and practices into everyday practice
3 Leaders show the way and light the path for others
4 Relationships aren’t a priority, they’re a prerequisite
5 Holding each other to account for behaviours, not just outcomes
6 The rule of the golden thread: not all improvement matters in the same way
For more articles on Healthcare and Wellbeing sign up to Core Insights here.




 X
X Facebook
Facebook LinkedIn
LinkedIn YouTube
YouTube Instagram
Instagram Tiktok
Tiktok