
Learning fast: The NHS partnership with the Virginia Mason Institute has created lots of new innovations
Since 2018, I’ve led the team from Warwick Business School that evaluated the partnership between the English National Health Service (NHS) and the Virginia Mason Institute (VMI) from the USA.
The goal of the partnership was to implement a systematic approach to quality improvement (QI) in five English hospital systems (NHS trusts) and to derive lessons about how to foster a culture of continuous improvement across the wider health and care system. Here, I summarise six key lessons from the evaluation report for health and care leaders looking to build a systematic approach to QI.
This partnership was the biggest and most ambitious experiment in organisation-wide improvement in the history of the NHS. It was set up in a spirit of 'failing forward' - with a collective learning culture in which opportunities to do things differently were proactively sought and failures, large and small were consistently reported and deeply analysed.
The recently published evaluation report reflects this ethos. It contains rich and detailed analysis of partnership outcomes, including discussion of what went well, the challenges faced, a quantitative assessment of outcomes, and most importantly what can we learn.
I have set each lesson out separately, but all of them are interconnected.
Lesson 1: Build cultural readiness as the foundation for better QI outcomes
While each of the five NHS trusts had implemented the same improvement method, at the same time, with the same resources, their journeys and their outcomes were notable for their differences.
The most important differentiating factor between the trusts was the level of cultural readiness to embrace new ways of working. Specifically, we found that where a hospital trust had engaged in ‘cultural work’ in the years prior to adopting a systematic approach to QI, the intervention had something to ‘plug into’.
We define cultural work as planned and deliberate efforts to establish and maintain a shared set of values that all organisational members can align to. At Leeds Teaching Hospitals NHS Trust (LTHT), the CEO engaged a crowdsourcing exercise to co-produce a set of values that everyone who worked in the trust could align to.
At Surrey and Sussex Hospitals (SASH) the CEO told us organisational priorities are directly linked to clinical values, and in every interaction with a clinician he makes it clear they should spend all their time on patient experience, quality and safety.
Michael Wilson said: “The patient is the one consistent thing everybody’s got in common. It’s the one reason why we’re all here and if you keep framing it that way, you can’t really lose.”
We know that culture doesn’t change in a day, but it can and does happen with focused activity that seeks to embed a shared set of values that are clear, concise, constant and meaningful to everyone.
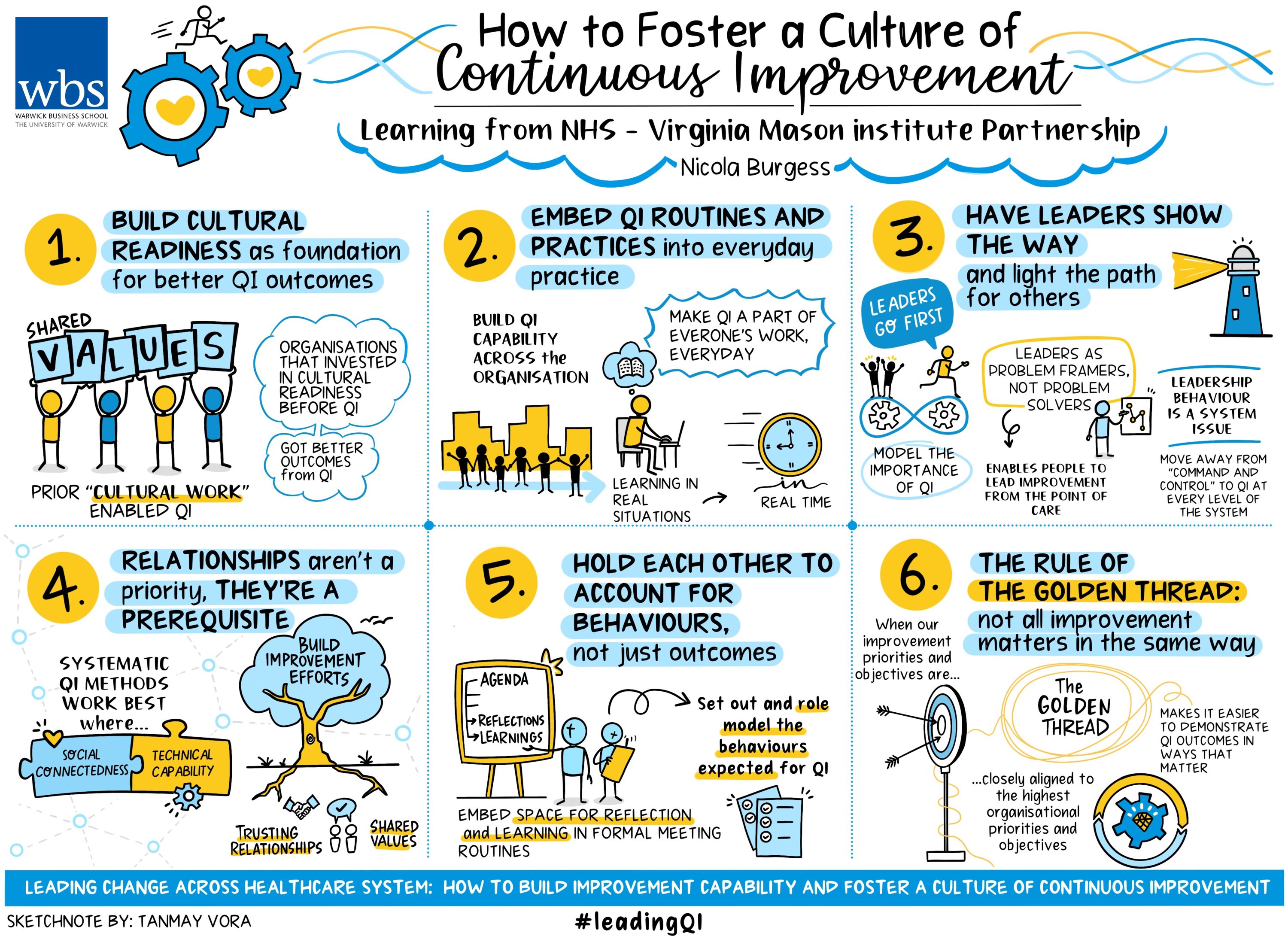
Lesson 2: Embed QI routines and practices into everyday practice
Organisational routines and practices that are clear, aligned and visible help to foster an unambiguous message about the organisation’s long-term commitment to patient-centred quality improvement and the role everyone has to play in making things better for the people who use the services and their families, every day.
Each of the five hospital trusts implemented a continuous improvement infrastructure comprising: internal strategic boards that met monthly to discuss QI; related priority setting, project management and monitoring of improvement activity; a central improvement team was implemented, and newly recruited improvement specialists received training and certification by experts from the VMI.
The role of the improvement team was to design, facilitate and monitor improvement activity aligned to strategic priorities, as well as facilitating a rigorous training programme known as ‘Lean for Leaders’ (L4L). The L4L training combined classroom and practical assignments across six modules, with improvement activity shared with senior leaders (usually the CEO) on a weekly basis.
L4L fostered the spread of daily management practices such as ‘huddles’, ‘production boards’ and ‘standard work’ that meant conversations about quality and improvement appeared everywhere every day.
As a side note, our analysis found the majority of financial savings derived from the partnership were classed as ‘training inspired’. In other words, improvement activity led by an employee who had completed L4L and subsequently led improvement activity within their teams and departments.
This demonstrates the importance of investing in improvement capability, then making that capability part of the everyday work of the organisation, learning in real situations in real time.
Lesson 3: Leaders show the way and light the path for others
The NHS-VMI partnership invested significantly in leadership training and coaching. L4L symbolised a focus on building the QI capability of health and care leaders, starting at the top of the executive tree and then opening up to middle level and frontline leaders.
Senior leaders who ‘go first’ are sending a message to others that participation is important. In line with lesson one, we found cultural readiness was positively correlated to senior leader engagement with L4L training.
For example, in one of the trusts where shared values were deeply embedded, executive leaders told of a palpable ‘excitement’ about the training ‘opportunity’, and a waiting list of leaders of all levels. By contrast, in a trust with less cultural readiness, long-standing cultural issues negatively impacted engagement.
Leaders should be problem framers, not problem solvers. The need to develop a new leadership style was a frequent reflection from the CEOs of the five participating trusts.
Moving from 'problem solver' to 'problem framer' can be hard when careers have been won on the basis of firefighting and problem-solving prowess. Despite this, leaders told us that a more facilitative problem-framing approach is “always more effective”.
Put simply, those who do the work know best how to improve the work; when a leader frames a problem, they give permission for employees to lead improvement from the front line.
Leadership behaviour is a system issue. Changes to leadership style are essential for developing an improvement culture within and across an organisation.
However, each organisation exists within a wider system. The efficacy of a coaching style of leadership can be rapidly undermined by a traditional, command and control approach to oversight and governance at a higher level of the system; in the current context, that is integrated care boards, regional and national bodies.
Lesson 4: Relationships aren’t a priority, they’re a prerequisite
Systematic QI methods such as the lean approaches promoted by the VMI are socio-technical. In other words, the implementation of lean relies upon individuals having technical capability and social connectedness.
For lean to be effective at delivering QI in a continuous and sustainable manner, you need both the skills of QI and the ability to inspire and collaborate with influential others.
One of the most striking outputs from the evaluation came from our social network analysis (SNA) of individuals who had completed the L4L.
Our objective was to understand what happens after training is completed. In other words, is QI knowledge shared and used to foster improvement or is the training perceived as a mere tick-box exercise, returning to business as usual once completed?
To our surprise the SNA graphs illustrated striking differences in the connectedness of employees between a trust rated ‘outstanding’ for performance, and one that had gone into ‘special measures’.
Both trusts were of a similar size, with similar numbers of employees trained in L4L. The difference: at the high performing trust, everybody was talking about improvement. At the lesser performing trust, relationships were predominantly non-reciprocal, indicative of a culture where interactions are of a ‘messenger’ type, and information is shared on a need-to-know basis.
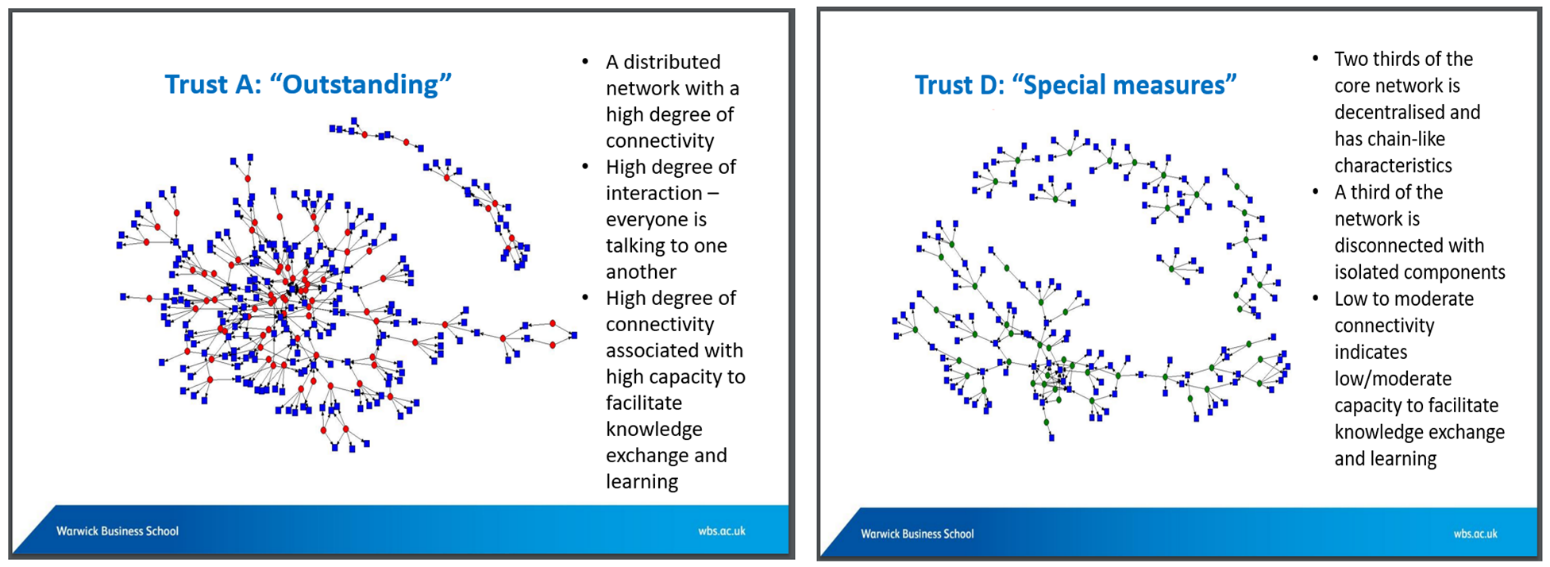
Hence, organisations must pay attention to the social aspect of QI and build their improvement efforts on foundations of strong relationships and shared values.
Lesson 5: Holding each other to account for behaviours, not just outcomes
Unique to the NHS-VMI partnership was a monthly meeting between all five CEOs and national leaders.
The meeting, known as the Transformation Guiding Board (TGB) took place in central London and was 5.5 hours long. Despite the lengthy duration and the exorbitant cross-country trek that each CEO made from their hospital to central London, this meeting was frequently referred to as "the best day of the month".
Usually, an all-day meeting between national bodies and a hospital CEO would signify an organisation under scrutiny, hence supplanting preconceived notions of the national leaders as something to fear was essential for effective partnership working. To foster this relational change, members of the TGB co-created a 'compact'.
A compact is an explicit (written) document that outlines the behaviours that each partner promises to uphold. The process of co-creating a compact is an important reflective exercise.
However, our analysis focused on how the compact facilitated and sustained new partnership ways of working, even when things weren’t going so well. A significant finding was the importance of routine activation of the compact.
Embedding ‘reflections on the compact’ into the monthly agenda of the TGB triggered conscious appraisal of the promises, goals and objectives that each partner pledged to enact and deliver. Subsequently, this ritual reflection built trust among the partners with frequent reassurance that each member remained committed to upholding the promises made.
Further, when behaviours were not aligned to promises established in the compact, the TGB became a safe space to ‘call out’ the breach, and openly discuss what went wrong and how to avoid it in the future.
Crucially, once the process of completing the compact is complete, its power for guiding relational change can only be realised if conscious and collective appraisal of the promises forms part of an established routine.
Lesson 6: The rule of the golden thread: not all improvement matters in the same way
A golden thread is present when organisational priorities and objectives align to improvement priorities and objectives.
In other words, improvement activity and specifically improvement objectives should be designed with higher level objectives in mind. Failure to define a ‘golden thread’ can mean improvement becomes hard to quantify in ways that matter.
Consider the differing approaches of the participating trusts. The trusts that had already built cultural readiness made strategic decisions at a senior leadership level about where the organisation should focus improvement activity.
As there was already a strong sense of shared values, it meant that the priorities of the improvement work and the overall goals of the organisation were aligned. This golden thread allowed the partnership work to be centre stage in the trust’s approach to continuous improvement.
By contrast, the trusts that didn’t have this foundation of cultural readiness adopted a ‘bottom up’ approach to selecting areas to focus improvement. Their rationale: “employee ownership…it’s that engagement piece.”
It meant that the topics selected for improvement were less likely to align with organisational priorities. When these trusts subsequently went into special measures, the performance improvement approaches and priorities associated with the performance recovery regime were different to the priorities determined as part of the partnership and it was hard to give centre stage to the partnership work.
The NHS-VMI partnership involved five NHS hospitals implementing the same methods, with proportionally same resource, during the same period.
Adopting a processual view of the outcomes and impact of the partnership for each of the five trusts presented a unique opportunity to develop deep understanding about what works, what doesn’t, and most importantly why (or why not). The findings are rich and compelling, offering important lessons for NHS leaders seeking to navigate challenges ahead.
I conclude by highlighting the important role of QI methods, tools and techniques during the COVID-19 pandemic. Despite the differential outcomes across the five NHS hospital trusts, we found all five used QI improvement methods extensively, and at every level of the organisation.
To illustrate, below is a quote from an NHS non-executive director, describing their observations of staff using QI methods to manage intense clinical demand at a time of heightened uncertainty and anxiety.
“We had command and control structures in place (like most other trusts) but the production boards, the huddles, the standard operating procedures and standard work that we’ve utilised as a result of the NHS-VMI partnership, those processes and principles really came to the fore.
“The daily huddle at eight o’clock in the morning really set the tone so we know who’s doing what…and there’s no duplication of effort…everybody knows what their role is in that incident room.”
To our surprise, at Barking Havering and Redbridge Hospitals Trust (where engagement with senior leaders and senior doctors had lagged during the partnership), the crisis gave the improvement system the legitimacy it had otherwise failed to achieve.
One Senior Manager said: “The Pride Way [improvement system] was central in the way that the trust dealt with the pandemic. But the pandemic has been central in getting the Pride Way into everywhere…”
Nicola Burgess is Reader of Operations Management and teaches Operational Management on the Distance Learning MBA plus Digital Innovation in the Healthcare Industry on the Executive MBA.
Follow Nicola Burgess on Twitter @DrNicolaBurgess.
Discover more articles on Healthcare and Wellbeing by signing up to Core Insights.




 X
X Facebook
Facebook LinkedIn
LinkedIn YouTube
YouTube Instagram
Instagram Tiktok
Tiktok